Infertility
Infertility is a disease of the reproductive system that impairs one of the body's most basic functions: the conception of children. Conception is a complicated process that depends upon many factors: the production of healthy sperm by the man and healthy eggs by the woman; unblocked fallopian tubes that allow the sperm to reach the egg; the sperm's ability to fertilize the egg when they meet; the ability of the fertilized egg (embryo) to become implanted in the woman's uterus; and sufficient embryo quality.
One in every six couples of childbearing age has a problem conceiving. Over 80% of all infertile couples can be helped to achieve pregnancy with proper medical treatment.
Infertility is a female problem in 35% of the cases, a male problem in 35% of the cases, a combined problem of the couple in 20% of cases, and unexplained in 10% of cases. It is essential that both the man and the woman be evaluated during an infertility work-up.
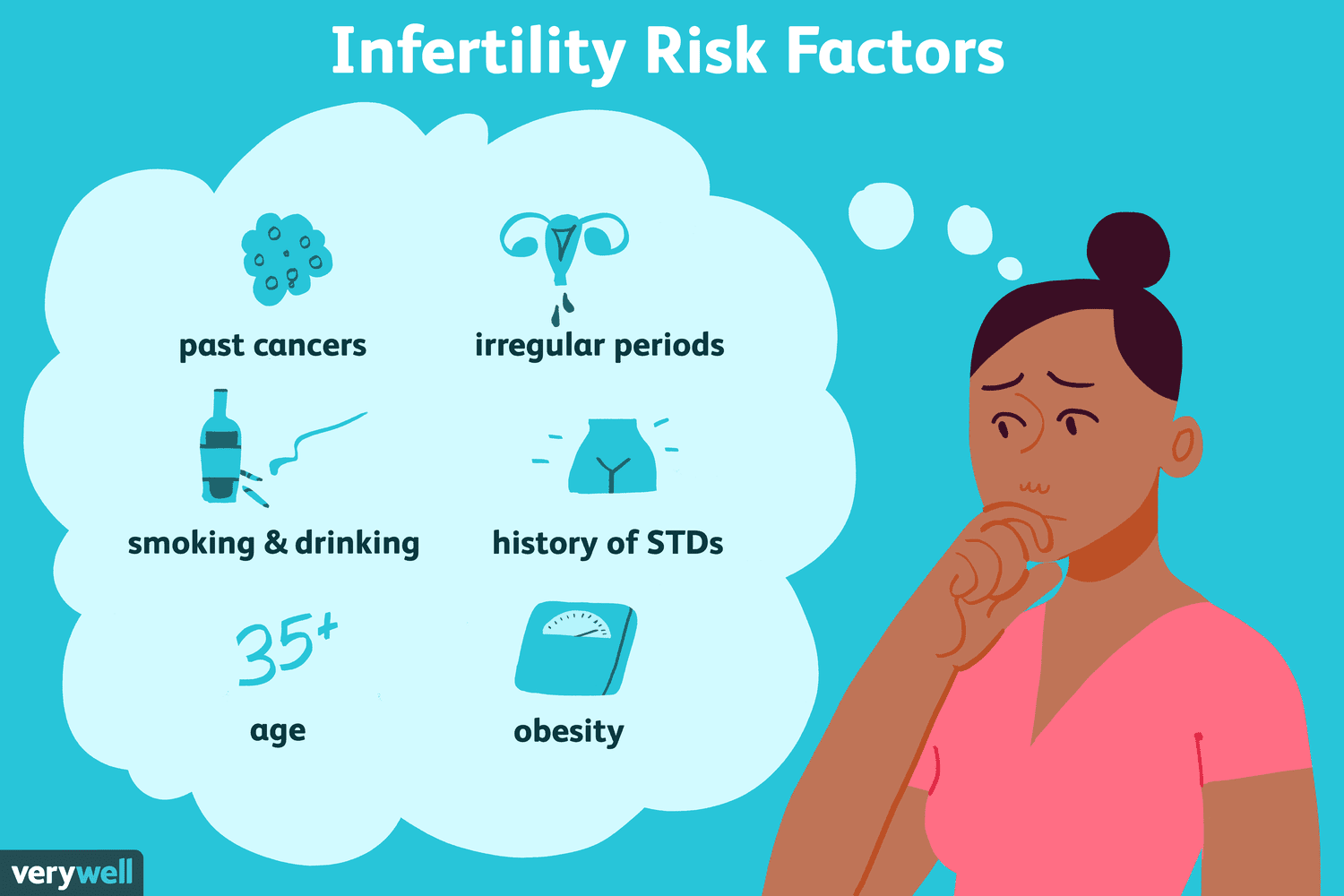
Most physicians advise you not to be concerned unless you have been trying to conceive for at least one year. If the female partner is over 30 years old and has a history of pelvic inflammatory disease, painful periods, recurrent miscarriage, or irregular periods then it might be prudent to seek help sooner. Waiting only 6 months before having an initial consultation for women 35 years and older is often recommended since if a problem is found there is less time for correction. If the male partner has a known or suspected low sperm count, then it would also be prudent to seek help sooner than waiting a year.
Problems with ovulation account for most infertility in women. Without ovulation, eggs are not available to be fertilized. Signs of problems with ovulation include irregular menstrual periods or no periods. Simple lifestyle factors – including stress, diet or athletic training – can affect a woman's hormonal balance. Much less often, a hormonal imbalance from a serious medical problem such as a pituitary gland tumour can cause ovulation problems.
Causes Of Infertility
What is an orgasm? An orgasm is an emotional and physical experience that occurs during a “sexual response cycle”. Before an orgasm, your body becomes increasingly excited. Breathing, heart rate and blood pressure increase.
With increasing intensity of the sexual stimulus, the reflex centres of the spinal cord begin to emit impulses that leave the cord to the genitals and initiate emission, which is the forerunner of ejaculation. Fluid from the vas deferens, the prostate, the ampulla, and the seminal vesicles (and even more tiny glands) are propelled into the internal urethra by contractions of the groin muscles*. The filling of the internal urethra elicits signals that are transmitted through the pudendal nerves from the spinal cord. Increases in pressure in the urethra cause the semen to be propelled to the exterior, resulting in ejaculation! The period of emission and ejaculation is termed male orgasm. After ejaculation erection ceases within 1 to 2 minutes in most males.
The male orgasm is not just about ejaculation. It is possible to have an orgasm without ejaculation. # Pre-adolescent boys can often experience an orgasm without ejaculation.
# Some men do not have an ejaculation until several seconds after orgasm.
# Other men who are incapable of ejaculation are still capable of orgasm.
# Adult males may experience several ejaculations and go on to have further orgasms without ejaculation.
Although many experiences have common ground there are differences too between the male and female orgasm.
The female orgasm has the effect of sucking sperm towards the female's egg,(the ovum) in the fallopian tube.
Women can often experience an orgasm for a longer period of time than a man.
Women are, in general, more capable of rapidly returning to orgasm immediately after an orgasmic experience.
Male Infertility
What are the most common causes of male infertility?
Varicoceles
Varicoceles are dilated veins in the scrotum, (just as an individual may have varicose veins in their legs.) These veins are dilated because the blood does not drain properly from them. These dilated veins allow extra blood to pool in the scrotum, which has a negative effect on sperm production. This condition is the most common reversible cause of male factor infertility and may be corrected by minor outpatient surgery.
Most experts do this microscopically to preserve the arterial supply and lymphatics. A sub-inguinal incision (about 1 inch above the penis and 1 inch from the midline) is usually used, as this avoids incising the abdominal muscles and creates less post-operative pain.
Abnormalities in the seminal fluid
If the seminal fluid is very thick it may be difficult for the sperm to move through it and into the woman’s reproductive tract. Often the semen can be processed to separate the moving sperm from the surrounding debris, dead sperm and seminal fluid. The processed sperm is usually placed directly inside the uterus with a small tube (catheter). This is called intrauterine insemination (IUI).
Problems with the ductal system
Sperm-carrying ducts may be missing or blocked.
A patient may have bilateral (both sides) congenital (from birth) absence of the vas deferens.
He may have obstructions either at the level of the epididymis (the delicate tubular structure draining the testes) or higher up in the more muscular vas deferens. He may have become mechanically blocked during hernia or hydrocele repairs. He may have become blocked by scar tissue as a response to an infection.
Sperm are stored in sacs called the seminal vesicles and are then deposited in the urethra which is the tube through which men urinate and ejaculate. The sperm must pass through the ejaculatory ducts to get from the seminal vesicles to the urethra. If these are blocked on both sides no sperm will come through.
In some situations the ducts may be repaired or unblocked, to allow them to flow through the man's reproductive tract. If this is not possible, the sperm may be harvested, to allow them to flow through the man's reproductive tract. But because they are obtained in lower numbers they must be used in conjunction with advanced reproductive techniques to attempt a pregnancy.
Immunologic Infertility
Men can develop an immunologic response, (antibodies) to their own sperm. The causes for this may include testicular trauma, testicular infection, large varicoceles or testicular surgery. Sometimes there are unexplained reasons why this occurs.
These antibodies have a negative effect on fertility although the exact reason why this is the case is unclear. Most likely these antibodies act negatively at several points along the pathway to fertilization. They make it more difficult for the sperm to penetrate the partner’s cervical mucous and make its way into the uterus. They make it more difficult for the sperm to bind with the zona pellucid (the external membrane or shell of the egg). Also, the antibodies make it more difficult for the sperm to fuse with the membrane of the oocytes (eggs) themselves.
The treatment for anti-sperm antibodies is somewhat controversial. Men may be treated with corticosteroids. However, this can lead to significant morbidity in the man. The most significant is aseptic necrosis of the hip (noninfectious destruction of the joint) requiring a hip replacement.
Most of the time, the first level of intervention includes intra-uterine inseminations. If the couple is planning invitro fertilization, (IVF) the presence of anti-sperm antibodies is usually an indication to inject the sperm directly into the egg (ICSI) instead of conventional IVF.
Difficulties with erections and ejaculation
About 5% of couples with infertility have factors relating to intercourse. This includes the inability to obtain or maintain an erection, premature ejaculation, lack of ejaculation, retrograde (backwards) ejaculation, lack of appropriate timing of intercourse and excessive masturbation. Interestingly, the most common problem is infrequency of intercourse. Many men will have difficulty with erections under the pressure at trying to achieve a conception. These couples can easily learn the technique of self inseminations. Studies have shown that 5 out of 6 previously fertile couples having intercourse four times per week will conceive over six months, while only 1 out of 6 with intercourse once per week will conceive during the same period.
Testicular Failure
This generally refers to the inability of the sperm-producing part of the testicle (the seminiferous epithelium) to make adequate numbers of mature sperm. This failure may occur at any stage in sperm production for a number of reasons. The testicle may completely lack the cells that divide to become sperm (“Sertoli Cell-Only syndrome”). There may be an inability of the sperm to complete their development (" maturation arrest"). Sperm may be made in such low numbers that few if any successfully travel through the ducts and into the ejaculated fluid (hypo spermatogenesis). This situation may be caused by genetic abnormalities, hormonal factors, or varicoceles.
Even in the case where the testes are only producing low numbers of sperm, the sperm may be harvested and used in conjunction with advanced reproductive techniques to attempt a pregnancy.
Cryptorchidism
Cryptorchidism may be a cause of testicular failure. When a baby boy is born without the testes having fully descended into the scrotum the condition is known as cryptorchidism.
Since the testes are very sensitive to temperature, if they do not descend into the scrotum prior to adolescence, then they will stop producing sperm altogether. In fact, they have a higher rate of malignancy. The current recommendation is that at approximately one year of life if they have not yet descended by themselves, they be brought down surgically.
Cryptorchidism is often associated with male factor infertility. 81% of men who have a single testis that is cryptorchid have normal fertility. However, approximately only 50% of men who have bilateral cryptorchidism have normal fertility. This may be due both to something inherent in the testes, to the surgery, or to the damage done by not having brought the testes down in time.
Drugs
There are a number of fairly common drugs, which may have a negative effect on sperm production and or function. They include:
Ketoconazole (an anti-fungal)
Sulfasalazine (for inflammatory bowel disease)
Spironolactone (an anti-hypertensive)
Calcium Channel Blockers (anti-hypertensives)
Allopurinol, Colchicine (for gout)
Antibiotics: Nitrofuran, Erythromycin, Gentamicin
Methotrexate (cancer, psoriasis, arthritis)
Cimetidine (for ulcers or reflux)
The following list of drugs can cause ejaculatory dysfunction:
Antipsychotics: Chlorpromazine, Haloperidol, Thioridazine
Antidepressants: Amitriptyline, Imipramine, Fluoxetine (Prozac), Paroxetine (Paxil), Sertraline (Zoloft)
Antihypertensives: Guanethidine, Prazosin, Phenoxibenzamine, Phentolamine, Reserpine, Thazides
Hormonal Abnormalities
The testicles need pituitary hormones to be stimulated to make sperm. If these are absent or severely decreased the testes will not maximally produce sperm. Importantly, men who take androgens (steroids) either by mouth or injection for bodybuilding shut down the production of hormones for sperm production.
A hormonal profile must be performed on all men with male factor infertility. This will help rule out serious medical conditions, give more information on the sperm-producing ability of the testes, and may reveal situations where hormonal treatment is indicated.
.jpg)
Infections
Men may have infections of their reproductive tract. These may include infections of the prostate (prostatitis), of the epididymis (epididymitis), or of the testis (orchitis).
Post-pubertal viral infections of the testes may cause significant damage (atrophy) to the testes and may cause absolute and irreversible infertility. Bacterial infections or sexually transmitted diseases may cause blockages in the sperm ducts. The patient may have normal production of sperm, but the ducts carrying it are obstructed.
Active bacterial or viral infections may have a negative effect on sperm production or sperm function. White blood cells, which are the body’s response to infection, may also have a negative effect on sperm membranes making them less hearty.
If excessive white blood cells or bacteria (more than 1 million/cc) are seen in a semen specimen, cultures should be done. This usually includes cultures for commonly asymptomatic, sexually transmitted diseases including mycoplasma, ureaplasma and chlamydia. Also, general genital culture is usually taken. If the infection and the white blood cells are persistent then antibiotics may be considered.
It is important to note that in most men the ejaculate is not sterile. In controlled studies, the average man will culture positive for approximately two organisms. It is therefore very important to be judicious in the treatment of non-sexually transmitted organisms found in cultures.
Genetic Abnormalities
When these conditions are treated, a man will often see a significant improvement in his semen analysis.
What lifestyle factors can affect sperm production?
Cigarette Smoking has been shown to significantly affect semen quality.
Regular smoking:
* causes a 23% decrease in sperm density (concentration) and a 13% decrease in motility (when averages are taken from nine separate studies). To a lesser extent, smoking causes an increased number of sperm with abnormal morphology (shape). Smoking causes toxicity to the seminal plasma (the fluid ejaculated with the sperm): sperm from non-smokers were adversely affected (had significantly decreased viability) when placed in the seminal plasma (hormonal) of smokers.
Smoking affects the hypothalamic-pituitary-gonadotropin axis, most commonly affecting levels of estradiol and estrone (estrogens, which are hormones found in higher concentrations in women). The Leydig Cells, which are in the testes and produce testosterone, may have secretory dysfunction. Most worrisome is that there is evidence that suggests that paternal smoking may also be associated with congenital abnormalities and childhood cancer, though the relative risk in most studies is less than two.
Recreational Drugs:
Marijuana (Cannabinoid)
often causes a decreased average sperm count, motility, and normal morphology. It affects the hormonal axis (HPG), causing decreased plasma testosterone. It may also have a direct negative effect on the Leydig Cells.
Cocaine, even infrequent cocaine use, causes decreased sperm counts, motility and normal morphology. These effects can be found in men who have used cocaine in the two years proceeding their initial semen analysis.
Cocaine also decreases the ability of sperm to penetrate cervical mucous, making it difficult for them to enter the uterus.
Anabolic Steroids (male hormones):
* The use of anabolic androgenic steroids has reached almost epidemic proportions. 6.6% of 12th-grade males use or have used them to build muscle mass and improve athletic performance. These male hormones suppress the testis' ability to make testosterone. This decreases the intratesticular testosterone level.
* They depress testicular production of testosterone and, thus, levels at testosterone inside the testes itself. This may cause severely diminished spermatogenesis or complete absence fo sperm (azoospermia).
* When taken, these steroids cause a persistent depression of the hypothalamus and pituitary which may be irreversible, even when the steroids are stopped.
Alcohol Moderate alcohol use does not affect male fertility. Excessive alcohol use
* Affects the hormonal axis and is a direct gonadotropin.
* It may cause associated liver dysfunction and nutritional deficiencies which are also detrimental for sperm production.
Lubricants
Most vaginal lubricants, including K-Y Jelly, Surgilube, and Lubifax are toxic to sperm. Couples should avoid their use during the fertile time of a woman's cycle.
Exercise
Moderate amounts of exercise can only be helpful. However, long-distance runners (men who run greater than 100 miles per week) and distance cyclers (men who ride greater than 50 miles per week) have decreased spermatogenesis. These activities should be moderated when a sub-fertile man is attempting to conception.
Infertility Treatment
Ovulation induction
A series of hormone injections will be given to the woman in order to stimulate egg growth and ovulation. If ovulation can be successfully induced, conception may then be able to occur naturally.
Artificial insemination
Artificial insemination is used in cases where the male has a low sperm count or a high number of abnormal sperm, or the woman has sperm antibodies present in her cervical mucus. Sperm is treated in the laboratory to increase the chances of fertilisation. Large numbers of sperm are then inserted directly into the uterus for easy access to the fallopian tubes.
IVF (In vitro fertilisation)
IVF is used to treat infertility blockages of the fallopian tubes, endometriosis, abnormal sperm, and some cases of unexplained infertility.
The woman is treated with hormones over a number of weeks to stimulate the growth of several eggs in the ovary. When ripe, the eggs are removed from the ovary and put into a dish with the partner's (or donor's) sperm. The fertilised eggs are then grown in the laboratory for a few days before being placed into the uterus.
For more detail on what's involved, see IVF.
GIFT (Gamete intrafallopian transfer)
This procedure is the same as that for IVF except that fertilisation takes place inside the body of the woman. The eggs and sperm (gametes) are collected and placed directly into the fallopian tubes for fertilisation to occur. GIFT is used in cases of endometriosis, cervical disorders, and some types of male infertility. It is suitable only for women with no abnormalities in the fallopian tubes.
ZIFT (Zygote intrafallopian transfer)
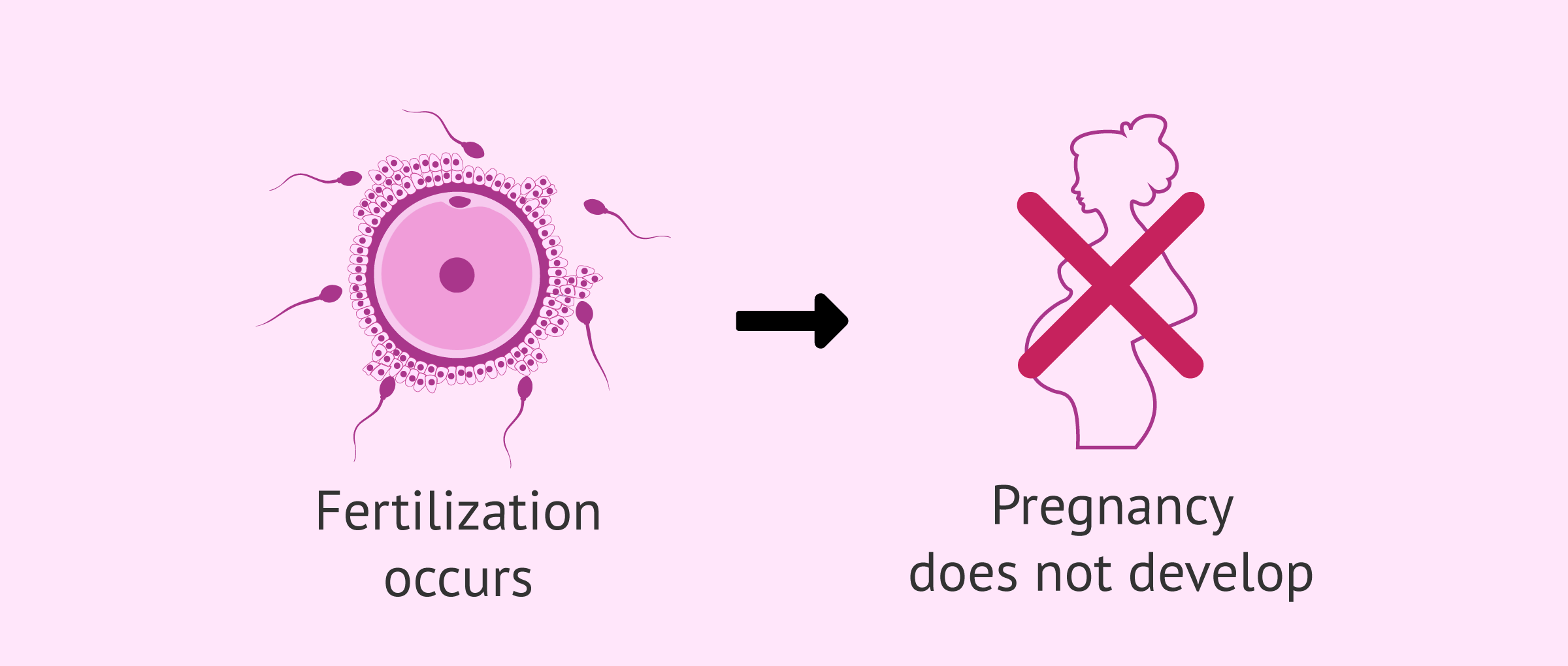
ZIFT involves the same procedure as IVF except that the very early embryo (zygote) is placed directly into the fallopian tube. This procedure is undertaken when there are abnormal sperm and/or problems with the ability of the sperm to fertilise the eggs.
ICSI (Intracytoplasmic sperm injection)
This is a technique in which a single sperm is inserted directly into the egg. Eggs are obtained the same way as for IVF and then fertilised by injecting a single sperm into them. The fertilised eggs can be transferred to the fallopian tubes of the woman or grown in the laboratory for a couple of days and then transferred to the uterus.
Epididymal and testicular sperm extraction
Sperm are removed from the epididymis or directly from the testis using a needle. Fertilisation is performed by ICSI (see above). This treatment is used in cases of male infertility such as azoospermia and spermatic cord abnormalities. Usually, enough sperm can be collected so that samples can be frozen for later use if required.
Freezing of sperm and embryos
If more embryos are produced through IVF than are needed for transfer into the woman's uterus, the extra embryos can be frozen. The stored embryos can be used later if the patient does not become pregnant, or if the couple wishes to have more children through IVF at a later date.
There is a limit to the number of years frozen embryos can be stored, and laws governing this may differ in each state (see Costs & legal issues).
Similarly, sperm can be frozen for use in subsequent IVF cycles, or as 'insurance' against infertility due to procedures such as cancer therapies, vasectomy or prolonged absence from a partner (such as men in military service may experience). Sperm can also be frozen and kept in sperm donor banks.
Donor eggs, embryos and sperm
For women who have an ovarian failure (see Types of Infertility), men who do not produce sperm or couples whose eggs fail to fertilise, the use of donor eggs, embryos or sperm may be an option. Older women may also wish to use donor eggs from younger women to overcome the problems of ageing.
Depending on which state you live in, there are certain legal restrictions on the use of donor eggs, embryos and sperm (see Costs & legal issues).
Pre-implantation genetic diagnosis (PGD)
PGD is an embryo screening technique that can be used to identify embryos with chromosome abnormalities. A single cell is removed from an early-stage embryo and checked for genetic disorders using molecular techniques. Only the healthy embryos are transferred to the woman's body.
Genetic disorders that can currently be detected in this way include cystic fibrosis, Duchenne muscular dystrophy, thalassemia, haemophilia A, muscular dystrophy, hydrocephalus, Huntington's disease, imbalances in the number of chromosomes (aneuploidy), and sex-linked disorders. Research is ongoing to develop reliable tests for other genetic disorders.

18 ways to make a baby
Natural sex
Artificial insemination -- of mother with father's sperm
Artificial insemination -- of mother with donor sperm
Artificial insemination -- with egg and sperm donors, using surrogate mother
In vitro fertilization (IVF) -- using egg and sperm of parents
IVF -- with Intra-Cytoplasmic Sperm Injection (ICSI)
IVF -- with frozen embryos
IVF -- with Preimplantation Genetic Diagnosis (PGD)
IVF -- with egg donor
IVF -- with sperm donor
IVF -- with egg and sperm donor
IVF -- with surrogate using parents' egg and sperm
IVF -- with surrogate and egg donor
IVF -- with surrogate and sperm donor
IVF -- with surrogate using her egg, sperm from baby's father
IVF -- with surrogate using egg and sperm donors*
Cytoplasmic transfer
Nuclear transfer and cloning
If you now add additional options such as TESA ( testicular sperm aspiration) and PESA ( percutaneous epididymal sperm aspiration);assisted hatching and embryo fragment removal, the list becomes even longer !
The bottom line is that today there is a solution for every infertility problem – and doctors and patients need to apply their mind, so they can decide what’s best for each individual couple !
The following herbs may be used to treat male infertility:
Ginseng (Panax ginseng)—Known as a male tonic (an agent that improves general health) and used to increase testosterone levels and sperm count. Siberian ginseng (Eleutherococcus senticosus) may also be used.
Astragalus (Astragalus membranaceus)—Increases sperm motility.
Sarsaparilla (Smilax spp.)—Known as a male (and female) tonic.
Saw palmetto (Serenoa repens)—Used for overall male reproductive health.
Other Recommendations
Avoid alcohol. Alcohol consumption is associated with an increased number of defective sperm. Consider acupuncture.
Do not smoke. There is an association between smoking and low sperm count, poor sperm motility, and abnormal sperm.
Semenax improves sperm count, concentration, and motility when taken orally for about 2 months. Approximately 30% of couples using it experience pregnancy. It is available without a prescription, although couples considering it should consult their physician.
Western herbalism
Several herbs effectively stimulate hormones necessary to fertility. Stinging nettle seeds contain estrogen-like phytohormones. Drink 3 cups of tea daily or add 1 tsp. of seeds to every meal. Prepare tea by adding 1 handful of seeds to 1 qt. of boiling water.
Red clover blossoms help restore and balance hormonal functions and nourish the uterus. The calcium and magnesium in the plant relax the nervous system and improve fertility. Red clover also balances the acid-alkaline level of the vagina which promotes conception. Combine with peppermint for flavor and sexual stimulation. Add 1 oz. of red clover blossoms and 1 tsp. of peppermint leaves to 1 qt. of boiling water. Steep for four hours. Strain and drink throughout the day for several months at a time. Wild raspberry leaf tea is an effective uterine tonic and contains a large amount of calcium. Drink 1 cup three times daily.
Lady's mantle strengthens the uterus lining, heals wounds and protects the mucous membranes. It inhibits spasms and regulates blood flow. Drink 10-15 drops of tincture in water three times daily.
St. John's wort blossom tea improves mood, calms, heals wounds and works as a nerve tonic. Pour 1 cup of boiling water over 2 tsp. of blossoms, Steep for five minutes, strain and drink.
Agnus castus acts on the pituitary gland to stimulate hormones involved in ovulation
False unicorn root stimulates the ovaries themselves and restores hormonal balance.
Wild yam is traditionally linked with the regulation of female hormones and the health of the reproductive organs. It contains a phytochemical that is a precursor of progesterone, the hormone that stimulates the uterus to prepare for pregnancy.
Rosemary helps maintain hormone balance.
German chamomile eases stress and promotes relaxation.
A dong quai combination formula, such as dong quai and peony or dong quai and bupleurum, help to strengthen the female hormonal system
Damiana, ginseng, gotu kola, licorice root, and blue cohosh are also good for women.
If the infertility is due to elevated prolactin levels or ovarian insufficiency, an extract of chaste berry (Vitex agnus-castus) can be helpful. The usual dosage of chaste berry extract (often standardized to contain 0.5 per cent agnuside) is 175 to 225 milligrams daily. It may take chaste berry extract a few months to produce its beneficial effects in restoring female balance. If a woman is ovulating, has no scarring, and still does not conceive, low thyroid function may be a factor.